Eating Disorders in General
Eating disorders are severe mental health conditions that impact individuals regardless of age, gender, ethnicity, or background. Those affected by eating disorders employ disordered eating behaviours as a means of managing challenging emotions or situations. These behaviours can encompass various patterns, such as restricting food intake, consuming excessive amounts of food in one sitting, engaging in harmful methods to purge food (e.g., self-induced vomiting, laxative misuse, fasting, or excessive exercise), or a combination of these actions.
It’s imperative to recognise that eating disorders are fundamentally rooted in emotions rather than solely focused on food itself. The individual’s relationship with food often serves as a coping mechanism or a way to regain a sense of control, even if they may not fully understand the underlying purpose of these behaviours. Importantly, it is essential to emphasise that the presence of an eating disorder is never the fault of the person experiencing it. Those affected by eating disorders deserve prompt and compassionate support to facilitate their recovery journey.
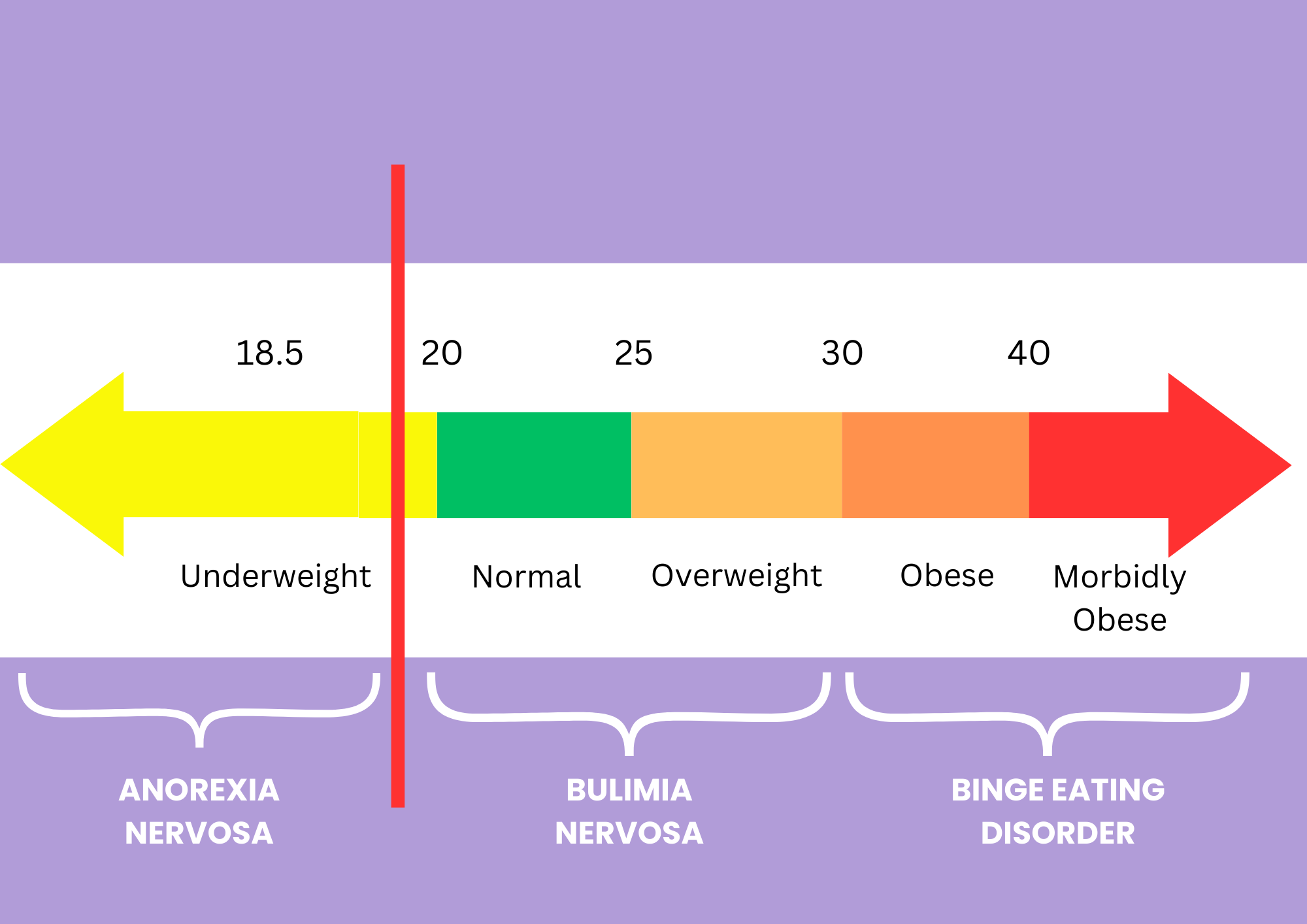
e.g. Eating Disorders Continuum and where they lie in relation to BMI (Body Mass Index) range. From what range is considered to be underweight, or normal range, through to morbidly obese. (Source: Allan S Kaplan, 2016)
Binge Eating Disorder: An Overview
In Australia alone, over one million people are currently living with an eating disorder, with binge eating disorder (BED) being the most prevalent among them. Of people with eating disorders, 47% have binge eating disorder compared to 3% with anorexia nervosa, 12% with bulimia nervosa and 38% with other eating disorders ().
Binge eating disorder is a serious mental illness characterised by recurrent episodes of consuming large quantities of food without feeling in control of one’s eating behaviour. This disorder can affect individuals of all ages and backgrounds and is more common than other eating disorders such as anorexia nervosa or bulimia nervosa. Unlike bulimia, people with BED do not typically engage in purging behaviours like vomiting, although some may fast between binge episodes. Most individuals with BED do not realise they have an eating disorder. Usually when they do seek help, it is usually for obesity treatment for weight loss or another condition.
Binge eating episodes are distressing experiences, often involving the consumption of far more food than a person would ordinarily desire. During a binge, individuals may struggle to stop eating, feeling disconnected from their actions or even unable to recall what they have consumed afterward.
Key Characteristics of Binge Eating Episodes
- Eating rapidly
- Eating until uncomfortably full
- Eating large amounts of food when not physically hungry
- Eating alone due to embarrassment about the quantity consumed
- Feelings of disgust, shame, or guilt during or after the binge
A person who experiences at least one of these distressing binge eating episodes per week for a minimum of three months is likely to be diagnosed with binge eating disorder.
The Complex Nature of Binge Eating
Binge eating episodes can take on various forms. Some may be meticulously planned, with individuals purchasing “special” binge foods, while others may be more spontaneous. People with BED may go to great lengths to access food, including eating discarded items or food that does not belong to them. Binge eating typically occurs in private, although individuals may have regular meals outside of their binge episodes.
Interestingly, some individuals with binge eating disorder may impose strict rules around food or engage in restrictive eating patterns, which can paradoxically lead to further binge eating episodes due to feelings of deprivation and hunger. The cycle of negative emotions, restriction, and subsequent binge eating can reinforce unhealthy eating behaviours.
Triggers for Binge Eating
Numerous factors can trigger the urge to binge eat, including emotional states such as sadness, shame, boredom, anger, stress, and anxiety. However, it’s essential to note that people may also engage in binge eating when experiencing positive emotions. Additionally, some binge eating episodes may be habitual or planned, rather than driven by sudden urges, often serving as a means to numb emotions or manage uncomfortable feelings, especially when an individual is alone.
Symptoms of Binge Eating Disorder
Binge eating disorder can have a profound impact on various aspects of an individual’s life. While not everyone with BED will exhibit the same symptoms, here are some common signs to be aware of:
Behavioural Signs:
- Excessive food purchases
- Organising life around binge eating episodes
- Hoarding food
- Rapid consumption of food
- Eating when not hungry
- Eating until uncomfortably full
- Avoiding eating around others
- Social withdrawal and isolation
- Irritability
- Mood swings
- Compromised education and employment plans
Psychological Signs:
- Constant preoccupation with food
- Feeling out of control around food
- Anxiety and tension, particularly when eating in front of others
- Low self-confidence and self-esteem
- Overwhelming feelings of guilt and shame after bingeing
- Comorbid mental health issues like depression or anxiety
Physical Signs:
- Fatigue
- Difficulty sleeping
- Weight gain
- Bloating
- Constipation
- Stomach pain
- Other gastrointestinal issues
- Poor skin condition
Long-Term Medical and Psychological Effects
Binge eating disorder, if left untreated, can lead to severe and even life-threatening consequences. Some of these long-term effects include:
- Obesity: Individuals with BED are at risk of becoming overweight or obese, which can contribute to various physical health risks.
- High blood pressure: Hypertension is a common comorbidity of BED, further increasing the risk of heart disease.
- High cholesterol: Elevated cholesterol levels are associated with BED, contributing to heart health concerns.
- Heart disease: BED can be a precursor to cardiovascular problems, making it crucial to address the disorder promptly.
- Type 2 diabetes: The link between BED and diabetes underscores the importance of early intervention.
- Fertility issues: BED can lead to difficulties conceiving and infertility.
- Joint and back pain: Excess weight gain can result in physical discomfort.
- Gastrointestinal problems: Frequent binge eating can damage the oesophagus and stomach.
- Arthritis: Obesity stemming from BED can exacerbate joint issues.
- Gall bladder disease: BED can increase the risk of gallbladder problems.
- Sleep apnoea: Obesity linked to BED can contribute to sleep apnoea.
- Social isolation: BED can lead to social withdrawal and isolation.
- Mental health issues: BED can contribute to or exacerbate conditions like depression, anxiety, self-harm, and suicidality.
- Distorted body image: Individuals with BED may struggle with extreme body dissatisfaction.
Causes of BED / Predisposing factors:
Genetic Influence – family history of eating disorders.
Environmental Effects – parental rearing style, religion, socioeconomic status
Sociocultural Factors –
- Family can be overprotective or too involved by providing a forgiving environment or Can magnify the culture pressure for thinness & stigma against overweight/obesity,
- Focus unduly on weight and shape and can potentially further damage a child’s self-esteem (such as professions or sports like ballet, gymnastics, modelling, figure skating, jockeying etc).
Media – tends to glorify eating disorders amongst actors and others in the public eye, like social influencers (2).
Treatment Options for Binge Eating Disorder
Thankfully, there are effective treatment options available for individuals with BED. Access to evidence-based treatment can significantly reduce the severity, duration, and impact of the disorder. The primary goals of BED treatment are to reduce binge eating episodes and support individuals in establishing regular eating patterns. Addressing co-occurring emotional factors such as anxiety, depression, and self-esteem is also crucial.
Psychological therapies that have proven to be effective in treating BED, including:
- Cognitive Behaviour Therapy Enhanced (CBT-E): This therapy focuses on identifying and modifying problematic thought patterns and behaviours related to binge eating.
- Cognitive Behaviour Therapy – Guided Self-Help (CBT-GSH): CBT-GSH is a self-help approach guided by cognitive-behavioural principles.
- Dialectical Behaviour Therapy (DBT): A type of therapy that focuses on teaching individuals’ skills to cope with stress and regulate emotions. Eating disorders, and in particular binge eating, fit this model nicely. We know that various eating disorder behaviours, like binge eating and purging, are often caused by negative mood states, including sadness, loneliness, frustration, and anger. This is because these emotions aren’t pleasant to experience, so people do the best they can to try to avoid or escape them. Binge eating offers this escape. Hence, DBT tries to teach people to implement better coping strategies and learn to tolerate distress.
- Interpersonal Therapy (IPT): IPT helps individuals explore and improve their interpersonal relationships, which can contribute to emotional well-being and reduced binge eating.
For most individuals, recovery from BED can be achieved through community-based treatment. A treatment team typically includes a medical practitioner, such as a general practitioner (GP), and a mental health professional, like a psychologist, trained in working with eating disorders.
In some cases, inpatient treatment may be necessary, particularly when individuals require medical or psychiatric stabilisation, nutritional rehabilitation, or more intensive support.
Medicare have available Eating Disorder Plans (EDP) that individuals can access, similar to Mental Health Care Plans. Many people in Australia who are experiencing eating disorders are able to access recovery support through Medicare.
The Eating Disorder Plan (EDP), is an evidence-based, best practice model of treatment. The plan can include up to 20 Medicare-subsidised sessions with a dietitian and 40 sessions with a mental health clinician over a 12-month period. An Eating Disorder Plan (EDP) referral can be obtained from your GP.
What can you do to assist in your recovery?
Tip 1: Develop a Healthier Relationship with Food
Recovery from binge eating begins with establishing a healthier connection with food. This means shifting from emotional eating to meeting your nutritional needs. Here’s how to break the binge eating cycle:
- Eliminate Temptation: Your chances of overeating skyrocket when you have junk food, desserts, and unhealthy snacks at home. Reduce these temptations by clearing your fridge and cupboards of your go-to binge foods.
- Maintain Regular Meals: Avoid the trap of waiting until extreme hunger strikes, as it often leads to overeating. Stick to your designated meal times to prevent binge eating later in the day.
- Listen to Your Body: Distinguish between genuine physical hunger and emotional cravings. If you’ve recently eaten and your stomach isn’t growling, chances are you’re not truly hungry. Allow the craving to subside naturally.
- Combat Boredom: Instead of succumbing to snacks out of sheer boredom, engage in distractions. Go for a walk, connect with a friend, immerse yourself in a good book, or explore hobbies like painting or gardening.
- Practice Mindful Eating: Break free from the trance-like state of mindless binge eating. Slow down and savour the textures and flavours of your food. Not only will you consume less, but you’ll also derive more enjoyment from your meals.
- Embrace Healthy Fats: Contrary to common belief, dietary fat can aid in curbing overeating and weight gain. Incorporate healthy fats into every meal to promote satisfaction and fullness.
The Importance of Avoiding Diets:
After a binge, the natural inclination is to diet and compensate for overeating. However, dieting often backfires, leading to food cravings and more binge episodes. Instead, focus on eating in moderation, enjoying nutritious foods, and avoiding strict food bans. Embrace occasional treats without guilt, rather than depriving yourself.
Tip 2: Address Emotional Triggers
Binge eating often occurs as an attempt to manage unpleasant emotions, such as stress, depression, shame, loneliness, fear, or anxiety. To tackle this aspect of recovery, follow these steps:
1. Learn to Tolerate Feelings:
It’s important to understand what feelings are triggered with BED –
• Identify the emotion you’re experiencing – take the time to try and clarify how you are feeling in the moment eg. anxiety, shame? etc
• Accept the emotion without judgment – and that often is really difficult to do. Being tough on yourself will only intensify the feeling. Try to be more compassionate towards yourself – “what would you say to a best friend who felt this way about themselves?”.
• Explore how it manifests in your body and your thoughts.
• Remember that emotions are temporary; they don’t define you.
Sitting with uncomfortable emotions is often challenging initially, but it’s a critical step towards overcoming binge eating.
2. Keep a Food and Mood Diary:
Maintain a diary to identify patterns behind your binge eating. Record what you ate, what triggered the urge, your feelings before, during, and after eating. Over time, patterns will emerge.
Tip 3: Manage Urges and Cravings
Binge urges can feel overpowering, but you can regain control. Here’s how:
- Distract Yourself: Engage in activities that capture your attention, like taking a walk or watching something entertaining. Once focused on something else, the binge urge may fade.
- Accept and Ride Out Urges: Don’t fight the urge to binge; instead, let it pass like a wave. This approach, known as “urge surfing,” can help the urge dissipate.
- Delay the Binge: Even if you’re unsure if you can resist, delay the binge. Start with a minute and gradually extend the delay over time. Often, this can help you avoid bingeing altogether.
- Talk to Someone: Share your feelings with a trusted friend or family member when you sense the urge to binge. Talking can alleviate the urge.
Tip 4: Support Yourself with Healthy Lifestyle Habits
A strong foundation of physical and emotional well-being can assist in resisting binge urges. Here are key lifestyle habits to support your recovery:
- Social Connections: Maintain close relationships rather than self-isolate – and engage in social activities to build a strong support network.
- Adequate Sleep: Ensure you get enough sleep each night to regulate appetite and reduce food cravings.
- Stress Management: Find alternative ways to cope with stress, such as meditation, sensory relaxation, and breathing exercises, to reduce reliance on food to ‘self-soothe’.
- Regular Exercise: Physical activity boosts mood, energy levels, and reduces stress. It can counter emotional eating.
Conclusion
Recovery from binge eating disorder is achievable with commitment, self-compassion, and the right strategies. By developing a healthier relationship with food, addressing emotional triggers, managing urges, and embracing a balanced lifestyle, you can regain control over your eating habits and lead a fulfilling life free from binge eating.
Understanding the causes, symptoms, and available treatment options is critical for supporting those affected by BED and promoting overall mental and physical well-being. If you or someone you know is struggling with binge eating disorder, don’t hesitate to seek help from a healthcare professional.
If you would like assistance, please don’t hesitate to reach out to us. 📞 Give us a call at (08) 9248 7852 or visit www.ndpsych.com.au to schedule an appointment 😊
References:
1 Hay P, Giorosi F, Mond J. Prevalence and sociodemographic correlates of DSM-5 eating disorders in the Australian Population. J Eating Disorders. 2015; 3(1): 1-7
2 Allan S Kaplan MD. Webinar: Understanding the Facts About Binge Eating Disorder – https://www.youtube.com/watch?v=-8CSDHzHLes&t=2816s
3 National Eating Disorders Collaboration NEDC – Binge eating disorder